Header logo
header top contact widget
Dental Implants
Gift Ideas For “Priceless” Smiles!
Posted on Sep 25, 2024 by William J. Claiborne, DDS MS
 It’s not even October and already I’m seeing holiday sales ads and decor. This comes across as pretty confusing when Christmas items are mixed into Halloween candy and skeleton costumes.
It’s not even October and already I’m seeing holiday sales ads and decor. This comes across as pretty confusing when Christmas items are mixed into Halloween candy and skeleton costumes.
However, Americans are wise to get a jump on the holidays since the rush of the Christmas season can become overwhelming. A long holiday shopping list can often be more manageable by jumping on early sales, saving time and money. Like every list, though, there is always that hard-to-buy-for person. At Biltmore Periodontics in Asheville, we have a suggestion…
An electric toothbrush can do a lot more than help an individual enjoy fresh breath and a bright smile. Studies have shown that brushing teeth with an electric version promotes better gum health and slower progression of periodontal (gum) disease. Compared to manual toothbrushing, an electric toothbrush can help to reduce the risk of tooth loss.
As part of a thorough at-home oral hygiene regimen, the thoroughness of an electric toothbrush was monitored in one study (published by the Journal of Clinical Periodontology). In this, the oral health of over 2800 adults was tracked for over 11 years. The use of electric toothbrushes was monitored to watch for periodontal disease, cavities, and the number of natural teeth.
From 2002 – 2006, participants were examined with follow ups conducted after 6 and 11 years. Eighteen percent of the participants were electric tooth brush users. At the time of their 11 year follow up, 37% had switched to using electric toothbrushes.
The study showed electric brushing promoted better gum health and slower progression of gum disease. Electric tooth brushing is also related to a reduction in tooth loss by 20% (compared to those who brush with manual toothbrushes).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6619286/
One reason for the superior level of cleaning by an electric toothbrush is attributed to features of some models. Many of the newer models include a timer to indicate how long to spend brushing in each quadrant (your teeth divided into 4 sections). The timers are also helpful in the recommendation of brushing for at least two minutes twice daily. (This applies to both manual brushing or with an electric.)
Gum disease is the nation’s leading cause of adult tooth loss and one of the most prominent diseases in the U.S., with over 47% of adults having some level. Signs of gum disease include tender gums that bleed easily when brushing, gums that darken in color to red (versus a healthy pink), persistent bad breath, and gums that pull away from teeth (receded gums) and expose darker root areas of teeth.
As devastating as tooth loss is, the infectious oral bacteria can enter the bloodstream through diseased gum tissues. They are able to create inflammatory reactions that have been associated with a long list of health problems.
Decades of research have shown the bacteria of gum disease are able to trigger the onset of or worsen the development of severe (and even deadly) health conditions. These include: heart disease, stroke, high blood pressure, some cancers, diabetes, arthritis, impotency, preterm babies, dementia, Alzheimer’s disease, and more.
Thus, the gift of an electric toothbrush to a smile you love can improve that person’s oral health and help them in their overall health as well! As a periodontist, I have a firsthand view at how these can help greatly when it comes to time spent at the bathroom sink!
Another gift suggestion is an electric water flosser.
 Daily flossing is highly recommended for gum health, lower cavity risk and the prevention of tooth loss. Flossing removes trapped bits of food remaining in the mouth, which feeds oral bacteria and allows them to quickly multiply. Because brushing cannot dislodge all food particles caught between teeth, flossing should be a must-do in one’s daily oral hygiene routine at home.
Daily flossing is highly recommended for gum health, lower cavity risk and the prevention of tooth loss. Flossing removes trapped bits of food remaining in the mouth, which feeds oral bacteria and allows them to quickly multiply. Because brushing cannot dislodge all food particles caught between teeth, flossing should be a must-do in one’s daily oral hygiene routine at home.
Proper flossing is easy for those who are in the habit and takes only a minute each day. While an estimated 40% of American adults “claim” to be daily flossers, that’s disputable. Some polls show that about 37% admit they actually floss less than daily with just over 32% saying they never floss.
https://www.usnews.com/news/articles/2016-05-02/how-many-americans-floss-their-teeth
For those who have problems with manual dexterity or find the maneuver awkward, water flossers are an effective alternative. They are easy to use and have been found to be just as effective as manual flossing.
A water flosser works by pulsating a stream of water between teeth that is forceful enough to dislodge trapped food bits but without harming teeth or gums. The pressure can also be adjusted for one’s comfort. They can be affordably purchased online or in many stores.
While adults are gaining a better understanding of how the health in their mouths impacts their overall help, we believe that – like anything – having the right tools can create a stronger commitment and positively support an individual in doing the job effectively. Because every smile gives back so much, protecting it – or helping someone protect theirs – is a gift that has lifelong benefits.
If signs or symptoms of gum disease are suspected, call 828-274-9440. If dental fear or anxiety is a concern, we can discuss comfort options, including oral and IV sedation (“twilight sleep”).
If regular dental care has been difficult for you in the past, consider starting with a consultation. You’ll find the entire team at our state-of-the-art Asheville periodontal dental office treat patients with respect, compassion and a gentle touch.
New patients are always welcome and referrals are not always required.
The Mirror Image Of Dental Implants
Posted on Sep 16, 2024 by William J. Claiborne, DDS MS
A study conducted in the United Kingdom in 2015 revealed that men check out their reflection 23 times a day while women do about 16 times. While other studies dispute the gender disparity (such as women using the mirror 34 times a day on average), all adults use the mirror more often than is probably perceived.
https://www.reuters.com/article/world/us/women-seen-checking-mirror-every-half-hour-idUSL05402197/
Naturally, part of that time in the mirror is spent each morning or evening as people prepare for the day and then get ready for bed. Ideally, several minutes of this time is being devoted to brushing and flossing. But, are they really getting a good look inside their mouths?
Typically, people don’t think all that often about the presence of their teeth, unless something hurts. Certainly, when hot or cold causes a sharp “jolt” of pain or a constant ache occurs around a particular tooth, an individual realizes something needs attention. After all, there is rarely pain in the mouth that is going to repair on its own. And, pain is our brain’s way of getting our immediate attention that something is wrong.
Adult tooth loss is fairly common in the U.S. Accidents, tooth (or tooth root) fractures, decay and certain health conditions can increase one’s potential for losing natural teeth. However, periodontal (gum) disease is the most common.
It is estimated that nearly half of the adult population have some form of periodontal disease (47.3%). Symptoms may include:
• tender and swollen gums that bleed easily when brushing
• persistent bad breath
• gums that are red in color rather than a healthy pink
• gums that recede from the base of teeth
• pus pockets around teeth as bacterial accumulate
• gums that are a spongy texture
• teeth that shift or loosen
According to the Centers for Disease Control & Prevention (CDC), over one-fourth (26%) of American adults ages 65 and older have 8 or less natural teeth. The CDC equates this number (having 8 or fewer teeth) as “severe tooth loss” since it impacts an individual’s ability to thoroughly eat a healthy diet.
 While losing a tooth during a lifetime seems “normal,” any loss of an adult tooth should be a wake-up call. As an Asheville periodontist, I know that losing a natural tooth can set into motion a snowball effect. And, it’s what occurs below the gums that creates the path that, for many older adults, leads to dentures.
While losing a tooth during a lifetime seems “normal,” any loss of an adult tooth should be a wake-up call. As an Asheville periodontist, I know that losing a natural tooth can set into motion a snowball effect. And, it’s what occurs below the gums that creates the path that, for many older adults, leads to dentures.
The absence of a tooth root in the upper or lower jaw bone is a loss of stimulation to the bone mass where it was once positioned. These roots provide both stimulation and nourishment that enables the bone to maintain a healthy mass. Without the presence of tooth roots, the bone begins to “melt away” in a process known as resorption.
It is commonly known that muscles, not used, will shrink in mass. When the jaw bones are lacking stimulation by the tooth roots they’re designed to hold, bone mass begins to shrink.
Resorption begins shortly after the tooth’s root is removed. Once it starts, it continues at an ever-increasing pace. For example, the first year after a tooth root is missing, bone decline may be minimal. With each passing year, however, the pace of bone loss accelerates.
As the bone shrinks in height, natural tooth roots adjacent to the area of missing teeth are subject to movement and root damage. On average, the next teeth you’re most likely to lose are the ones bordering areas of missing teeth.
How do you halt the process of tooth loss due to bone resorption?
Because dental implants replace the tooth above the gum line AND the root portion below it, the bone is able to retain its mass. Using the sturdy foundation of the jaw bone, dental implants are able to restore the look, feel and chewing stability like that of natural teeth.
A periodontist has advanced training to properly diagnose and treat all stages of periodontal (gum) disease (including gingivitis and periodontitis) as well as placement of dental implants. Because we understand the issues that occur above and below the gums, we are proponents of replacing teeth with dental implants, for a wide number of reasons.
1. Dental implants help to prevent declining mass of the jaw bone. In addition to problems associated with dental prosthetics (dentures, partials) when it comes to biting and chewing, bone loss causes changes in facial appearance that are aging far beyond one’s actual years. An implant restores stimulation to the bone and halts the progress of bone loss.
2. Dental implants have one of the highest success rates of any in-bone implant in the body, including hips and knees. When properly selected, placed and maintained, they are designed to last your lifetime.
3. Unlike crown-&-bridge combinations or partials, dental implants do not rely on neighboring teeth for support by adjacent teeth. And, because they help to preserve the bone that supports neighboring teeth, they are actually beneficial to the life of other natural teeth.
4. Dental implants are a one-time expense. They do not decay, require root canals, crack or break, future expense for upkeep or repairs is not needed. The material they are made of (titanium) biologically integrates with living bone and is not rejected nor will it cause adverse reactions to surrounding structures. With proper care, they will last throughout your life.
5. Because dental implants are supported by the upper or lower jaw bone, just as natural tooth roots, they are able to restore biting strength and chewing stability. After an implant is placed in the bone, the bone grows around it to fully secure it in the jaw. This enables confident biting and chewing without fear of movement that is possible with a denture or partial.
Like anything that is implanted into your body, dental implants should be placed in the hands of an experienced specialist. Ideal diagnosis is important, and can even save the patient in overall treatment costs. For example, when missing more than one tooth in one area, one implant can often hold two or a bridge of teeth. Several strategically-placed implants may also be used to support a full arch of teeth.
Proper placement and support in caring for implants is an important part of a successful outcome. However, dental implants can fail. A periodontal specialist can be an asset to your investment. When dental implants are chosen and placed by a periodontist, he or she is trained to select the one that will work best for you now and throughout your lifetime.
In addition to our specialized skills, our Asheville periodontal dental office provides advanced technology and a compassionate approach to care so you can enjoy a comfortable, efficient experience that allows you to have optimal success. Some of this technology is specific to dental implants, including: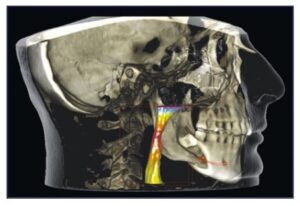
• LANAP With PerioLase MVP 7 – Laser-Assisted New Attachment Procedure is an advanced protocol that efficiently and effectively treats advanced gum disease with the added advantages of a dental laser. For patients who are preparing for dental implant placement, resolving gum disease prior to treatment is mandatory. LANAP offers a non-surgical alternative for patients with moderate to severe periodontal disease with very little discomfort and a quick recovery time.
• Cone Beam Imaging – These provide 3D images that are ideal for diagnosing and treatment planning. The highly-detailed images show sagittal, axial, and coronal planes, which locates and tracks nerve canals to optimize implant placement.
• Computerized Dental Implant Placement – This system provides the futuristic ability to position dental implants before the process actually begins. Through computerized technology, the implants are selected and “ideally positioned” on a 3D model of the patient’s jaw. From this, a template is developed for optimal treatment success, even for complex cases.
• CS 3600 Intraoral Scanner – Rather than make impressions with bulky, goopy trays, this scanner quickly and comfortably captures digital impressions accurately and easily. These are used to create precision models or appliances (dental implant crowns, bridges, or full arches). The scanner can also reach hard–to–access areas in the patient’s mouth for superior results with improved patient comfort.
For individuals who have lost teeth because dental fear or anxiety kept them from receiving regular dental care, we are especially sensitive to the concerns of these patients. Our entire team is committed to optimal patient comfort at every visit. Additionally, we offer:
• Oral sedation is a pill that helps patients relax. It also has an amnesiac effect, leaving most with little or no memory of treatment afterward.
• I.V. sedation (also known as “twilight sleep”) places the patient in a deeper sleep state and erases memory of the procedure. It is administered by a Medical Doctor (MD) who is a board certified Anesthesiologist.
For those who feel dental implants are out of reach financially, we encourage them to have a consultation to see exactly what their options may be and the treatment fees entailed. We offer several excellent payment plans, some with no down payment and no interest charged when paid according to the terms.
If you are considering dental implants, you may wish to begin with a consultation appointment. During this time, we can explain the vast difference in comfort, treatment time, and success available through our specialized skills and extensive technology.
Call 828-274-9440 to schedule. New patients are always welcome and a referral is not always required.
A Periodontist Is Your “Go-To” For Healthy, Beautiful Smiles
Posted on Sep 04, 2024 by William J. Claiborne, DDS MS
Children seem to know something adults don’t: Research shows that children smile an average of 400 times per day, compared to the average “happy” adult who smiles 40-50 times per day while the typical adult smiles only 20 times per day.
While a beautiful smile can make us more confident in how we appear to others, it also has health benefits you may not realize. According to Henry Ford Health, smiling can:
• Boost mood by causing the release of cortisol and endorphins
• Reduce blood pressure
• Increase endurance
• Reduces pain
• Reduces stress
• Strengthens immune system
In the article, they also share that studies show people who smile are perceived as more likable, courteous and competent. Smilers are also seen as more productive at work and are higher earners.
https://www.henryford.com/blog/2017/10/health-benefits-smiling
A pleasant smile is considered a symbol of beauty and well being. The appearance of a smile is influenced by a variety of factors including the shape and position of teeth and surrounding gum tissue levels. In cases where the gum tissues can greatly enhance esthetics, people often seek out the advanced skills of a periodontal specialist for periodontal plastic surgery.
Many general dentists and other dental specialists refer their patients to a periodontist for their specific skills. A periodontist is a dental specialist who is the expert in caring for the gum tissues. This includes all levels of periodontal disease as well as in the reshaping of gum tissues.
Crown Lengthening:
When the enhanced appearance of a smile is being sought, a periodontist is the pro in creating a balanced smile line. In the procedure known as “crown lengthening,” the arch of gum tissues over teeth visible in a smile can be repositioned. This is done in a procedure known as a gingivectomy.
In smiles that have an uneven line of gum tissues, the up-and-down line of tissue creates a jumbled look. Crown lengthening can alter the height of the gum arches over teeth, typically performed prior to placement of crowns (“caps”) to provide a more balanced smile line.
A crown lengthening procedure can sometimes save a tooth from removal, particularly when a tooth breaks near the gum line. By exposing more of the tooth’s structure, it may be possible to place a crown over the remaining tooth. This can help the patient avoid the extensive costs and potential upkeep of replacing it.
“Gummy” Smile:
Esthetically, a balanced smile typically shows the front top 6 or 8 teeth. Arching each tooth, there is generally minimal gum tissues showing, and sometimes none.
A gummy smile, in the periodontal specialty, is known as EGD, an abbreviation for excessive gingival display or a gingival smile (GS). The trait occurs more often in females than in males. (Gingival is of or relating to the gums.)
For individuals who have a “gummy” smile, it can be seen as a personal trait that many feel is a positive part of their individuality. A famous gummy smile is that of Katie Couric, who shares hers openly and beautifully.
However, not everyone with this trait feels comfortable with the look nor the way it makes them feel when smiling. Some people tend to suppress smiling fully. Others conceal their smile with a hand when smiling fully or laughing or “hold back” by smiling with their lips only.
A periodontist can determine the proper amount of gum tissue for your individual smile and provide contours that are natural and flattering to teeth. Because a periodontist is respectful to the care of tender gum tissues, they are the go-to of many general dentists when it comes to ideal and gentle treatment. This also helps in minimizing healing time.
Receded Gums:
Another procedure a periodontist expertly performs is gum grafting. This is often performed to cover exposed roots, reduce further gum recession, protect vulnerable tooth roots from decay, and improve your smile. Recession can occur as a result of periodontal disease, which causes tooth roots to become exposed and makes the teeth look long.
Gum tissues are very tender tissues with many nerves. Procedures that involve the gums must be performed with precision to minimize discomfort and speed healing time. A periodontist excels in the skills to create an optimal outcome with the most conservative treatment needed.
Replacing Teeth:
When tooth loss has occurred (whether from gum disease, an accident, or due to genetics), our Western NC periodontal dental office also works with a number of dentists in the diagnosis and placement of dental implants.
With over 40 different implant systems, the one suited best for you depends on factors that an experienced dental specialist takes into consideration. His or her skills in placement – achieving optimal angles and depths – helps to maximize treatment outcomes while enhancing comfort.
Patient Comfort:
Patient comfort has always been a high priority in our our Asheville periodontal practice. We are widely known for an environment of compassionate and respectful care and understand that over 70% of the adult population have some level of dental fear or anxiety. After all, we would want such an approach to care for ourselves and our loved ones.
For optimal comfort and relaxation, we offer several sedation options, including oral and IV sedation.
• Oral sedation is a pill that helps patients relax. It also has an amnesiac effect, leaving most with little or no memory of treatment afterward.
• I.V. sedation (“twilight sleep”) places the patient in a deeper sleep state and erases memory of the procedure. It is administered by a Medical Doctor (MD) who is a board certified Anesthesiologist.
With both sedatives, patients are closely monitored with advanced safety equipment throughout treatment.
In addition to advanced skills, our Asheville periodontal dental office is known for utilizing some of the industry’s most advanced technology, including LANAP Protocol using PerioLase MVP-7. This laser efficiently and effectively treats periodontitis (advanced gum disease). It causes very little or no discomfort and has a quick recovery time. This laser has also been found to stimulate bone regrowth in damaged areas.
Affordable Treatment:
We believe that every individual can live a happier, longer life with a healthy smile they enjoy sharing. If financial constraints are holding you back, ask about our easy payment plans. Most of these break treatment fees into monthly payments that are manageable to most budgets. They are interest-free and require no down payment.
Get the coming year started with your smile goals achieved! Call 828-274-9440 to schedule a consultation or exam at our Asheville periodontal dental office. Our friendly staff can help you arrange this private time together and will make you feel welcome.
Don’t Let Tooth Loss Make You LOOK or FEEL Old.
Posted on Aug 26, 2024 by William J. Claiborne, DDS MS
I have never imagined how old I could look until the first timerI saw my image on FaceTime. It reminded me of a time I unexpectedly passed by a mirror and saw an old man looking at me, which of course was my reflection.
Aging is tough enough without looking or feeling old. While adults have gotten better at staying more active and eating better diets than some previous generations, having an aged appearance beyond one’s actual years is a downer.
Something people often do not factor into the telltale signs of aging is bone loss. Generally, people acknowledge that they’ll lose some height with age as the skeleton submits to typical bone loss. However, bone loss due to missing natural teeth isn’t typically perceived as part of the process.
Yet, losing bone mass in the jaws can greatly affect one’s appearance, regardless of their actual years. This is due to the lack of stimulation provided to the jaws that natural tooth roots once provided.
Your natural teeth are supported by your upper and lower jaw bone, known respectfully as the maxilla and mandible. These strong, study bones support tooth roots securely.
When a natural tooth is removed, its absence causes a reaction below the gum line. This is through a process known as “resorption.” Without tooth roots present in the bone, the stimulation and nourishment needed for the bone to maintain a healthy mass is removed. Thus, the bone begins to decline.
As it shrinks in height, the adjacent teeth are more vulnerable to loss. Statistics show that teeth adjacent to areas where natural teeth are missing will be the most likely to be lost next.
Resorption begins shortly after the tooth root is removed. Once it starts, it continues at an ever-increasing rate year after year. For example, the first year after a tooth root is absent, the loss of bone may be minimal, probably unnoticeable. With each passing year, however, the pace of loss accelerates.
Over time, resorption’s effects become visible. As the bones decline in mass, deep wrinkles form around the mouth. The corners of the mouth turn downward. The chin takes on a more pointed shape and the mouth sinks into the face. The nose seems to get closer to the chin as the jaw bones thin. Jowls form as facial muscles detach from shrinking bone structure.
For people who wear a denture or partial, the pressure of wearing these appliances can speed up the rate of bone loss. For those who sleep in their denture, the 24/7 pressure speeds this pace even further. Even people who have a “bridge” may start to notice a space between the bridge and the gums, one that was probably not obvious before.
As a periodontist, I specialize in the prevention, diagnosis, and treatment of all stages of periodontal (gum) disease. In addition, periodontists are particularly skilled in performing cosmetic periodontal procedures. I also have advanced training and skills in the selection and placement of dental implants.
When it comes to replacing natural teeth, dental implants are the ideal for many reasons. When it comes to halting bone loss, they are able to restore stimulation to the jaw bone. Additionally, dental implants restore the ability to eat with stability, chew comfortably, and laugh and speak with confidence. Dental implants do not decay and will never need root canals.
There are over 40 different implant systems, each designed to accommodate various needs and goals. Obviously, a strong consideration in determining which type of dental implant is recommended is in the amount of jaw bone mass present.
An implant needs a particular amount of bone structure to support it. Depending on the amount of bone present to support the implant(s), the choice of which implant system to recommend can be made.
For some, we may recommend a bone rebuilding process prior to implant placement. Or, we may advise an implant that uses unique implant lengths and placement angles (the “All-On-4”) that can overcome the challenges of bone loss.
While there are also many considerations in selecting the right type of dental implant, the final choice, of course, is the patient’s preference. Does he or she want an implant that is non-removable (“fixed”)? Is cost the determining factor? Does the patient need just one implant or several? Can one implant dependably support a “bridge” of teeth in one area?
All in all, however, dental implants are an excellent choice for replacing teeth. Implants have an extremely high success rate, higher than any implant-in-bone option. And, dental implants are designed to last a lifetime. With proper selection and maintenance, they will never need replacing or repair.
Our Asheville periodontal practice is known for its priority on comfort and providing respectful care. With over 70% of the adult population having some level of dental fear or anxiety, we have a long-standing reputation for compassion and understanding.
For optimal comfort and relaxation, we offer several sedation options, including oral and IV sedation. With both sedation options, patients are closely monitored with advanced safety equipment throughout treatment.
• Oral sedation is a pill that helps patients relax. It also has an amnesiac effect, leaving most with little or no memory of treatment afterward.
• I.V. sedation (“twilight sleep“) places the patient in a deeper sleep state and erases memory of the procedure. It is administered by a Medical Doctor (MD) who is a board certified Anesthesiologist.
Ideal diagnosis is another important aspect of care here, which can save the patient much in overall treatment costs. For example, when missing more than one tooth in one area, one implant can often hold two or a bridge of teeth. Several strategically placed implants may also be used to support a full arch of teeth.
To support diagnostics in our Western NC periodontal dental office, we feature some of the region’s most advanced technology in the industry, including Cone Beam 3D imaging and laser dentistry. Our dental implant patients also have the advantages of technology that can minimize treatment speed healing and enhance comfort, thanks to Simplant.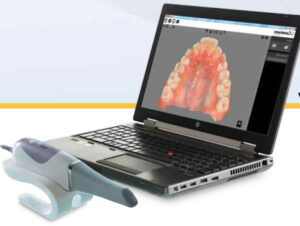
With the support of Simplant computerized dental implant placement, we can actually position the implants on the computer using a 3D model of the patient’s jaw pre-surgically. This aids in the selection of the implant type that ensures a precision fit.
For individuals who have lost a great deal of bone and need bone rebuilding procedures prior to placement, we are highly skilled in the procedures of bone grafting. However, in many cases, we are able to apply bone generation material to the area that is less involved than the grafting process.
We believe that proper placement and support in caring for implants is an important part of a successful outcome. However, dental implants can fail. This is why a periodontal specialist can be an asset to your investment. When dental implants are chosen and placed by a periodontist, he or she can select the one that will work best for you now and throughout your lifetime.
In our Asheville periodontal dental office, we combine technology with our advanced skills and compassionate approach to care so you can enjoy a comfortable, efficient experience that allows you to have optimal success.
Call 828-274-9440 to arrange a consultation. During this time, we can discuss treatment that can achieve your needs and goals as well as the process and anticipated costs. If interested, we will also explain payment plans, some that are interest free and require no down payment.
Recent Posts
Categories
Archives
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- July 2014
- June 2014
- May 2014
- April 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- June 2012