Header logo
header top contact widget
Blog Archives
Recent Posts
Categories
Archives
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- July 2014
- June 2014
- May 2014
- April 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- June 2012
How Periodontal Health Affects Your Overall Health
Posted on Apr 28, 2022 by William J. Claiborne, DDS MS
There are many benefits to having a clean, healthy mouth… fresh breath, bright teeth, avoiding cavities and preventing periodontal (gum) disease. However, much research shows that the health of your mouth can also affect your overall health to a rather significant extent.
Over the years, numerous studies have been able to pinpoint how certain diseases, such as coronary artery disease, diabetes, arthritis, etc. can be triggered. While there is still much to learn with some of these, the origins often point to internal (or “systemic”) inflammation.
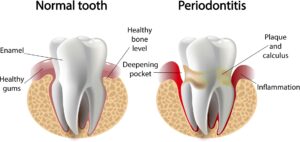
Inflammation in the body has been shown to set actions into play that cause the onset or worsening of a wide variety of health problems. Periodontal disease is a chronic inflammatory disease. This means the bacteria that attack tooth enamel and gum tissues are in a consistently active state.
When the bacteria of gum disease enter the bloodstream (through tears in weakened gum tissues), it can create inflammatory triggers far beyond the mouth. This bloodborne inflammation, in turn, results in higher risks for heart disease, stroke, diabetes, preterm babies, arthritis, respiratory diseases and even impotency.
To clarify, inflammation is not necessarily a bad thing. It’s the body reacting to an overload of bacteria. For example, the redness or slight swelling you see as a cut heals is a sign that the body’s defense system is fighting off bacteria that could create infection.
In chronic inflammation, however, the body’s defense mechanism becomes stuck in the ‘on’ position. This sets into motion a chain of reactions that transform a beneficial response into a harmful one. When an area in the body that stays in an inflammatory setting, there is a risk for damaging reactions.
One of the first correlations between oral bacteria and other serious health problems was found in heart disease. According to information published by the Harvard Medical School:
“In people with periodontitis (erosion of tissue and bone that support the teeth), chewing and toothbrushing release bacteria into the bloodstream. Several species of bacteria that cause periodontitis have been found in the atherosclerotic plaque in arteries in the heart and elsewhere. This plaque can lead to heart attack.
“Oral bacteria could also harm blood vessels or cause blood clots by releasing toxins that resemble proteins found in artery walls or the bloodstream. The immune system’s response to these toxins could harm vessel walls or make blood clot more easily. It is also possible that inflammation in the mouth revs up inflammation throughout the body, including in the arteries, where it can lead to heart attack and stroke.”
http://www.health.harvard.edu/press_releases/heart-disease-oral-health
Another good example is in the similarities between the tissues of gum disease and those taken from arthritic joints (another inflammatory disease). For decades, it was perceived that RA (rheumatoid arthritis) patients had such a high risk of gum disease due to poor oral hygiene because of dexterity problems with using a toothbrush. However, continued studies showed that gum disease is actually a risk factor for arthritis.
And, it was found that one can contribute to the other. Gum disease is a risk factor for developing RA and having arthritis patients have a greater risk for gum disease.
While genetic factors certainly contribute to greater RA susceptibility, the true source has been determined to be inflammatory reactions. This inflammation is triggered primarily by bacterial infections and the list of damaging outreach of oral bacteria seems to get longer and longer.
Studies have shown that pregnant women with periodontal disease have a greater risk of having pre-term and low birth weight babies. These indications have been found in amniotic fluid and in fetal cord blood samples of infants.
Also alarming is research that revealed that the bacteria of periodontal disease may contribute to a higher risk of pancreatic cancer. For years, researchers at the National Cancer Institute and the American Cancer Society have conducted a cancer prevention and screening study.
By studying oral samples, notably higher levels of two types of oral bacteria were measured in study participants with pancreatic cancer. One oral bacteria was found to create a 50 percent increased risk for pancreatic cancer and the second oral bacteria led to a 59 percent greater likelihood.
Chronic inflammation, in any area of the body, is a health risk that poses severe challenges. Not surprisingly, we occasionally see patients who have been advised by their surgeons to have their gum health checked prior to surgery. This proactive measure is to reduce risk factors that could complicate surgical outcome.
If you have symptoms of gum disease, please be seen by a periodontist promptly. Symptoms include tender gums that bleed easily when brushing, frequent bad breath, swollen and tender gums and gums that redden in color from a healthy pink. Remember, gum disease will only worsen without treatment and is the nation’s leading cause of adult tooth loss.
Maintaining good at-home care of your oral health is easy and takes just minutes a day. Follow a thorough oral hygiene regimen by brushing twice a day (two minutes each time) and floss daily. Drink plenty of plain water throughout the day and limit sugar. Have dental cleanings every six months and follow your dental hygienist’s recommendations to keep oral bacteria at minimal levels between visits.
If you suspect you have gum disease or have delayed (or avoided) having regular dental care, call our Asheville periodontal dental office to schedule an examination. Or, ask to begin with a consultation appointment. During this time, we can discuss any concerns and I’ll gladly answer any questions. Call 828-274-9440.
Dental Implants – Lower Risks Of Failure With These Tips
Posted on Apr 21, 2022 by William J. Claiborne, DDS MS
In our Asheville periodontal dental office, we believe our patients appreciate being fully informed about their oral health status and understanding their options for treatment. For those who have lost natural teeth, our specialty dental services include the diagnosis and placement of dental implants.
The specialized skills of a periodontist provides implant patients with a high level of success in treatment outcome. It also offers patients a wider variety of choices when it comes to implant systems.
This is why many general dentists who offer dental implants refer the placement portion to a periodontal specialist. For their patient, this can mean a higher level of success, especially for complex needs.
For example, a patient who is missing a lot of bone mass (often due to missing natural teeth for many years) benefits from the specialized skills of our Asheville periodontal office. Another example is a patient who has lost teeth due to periodontal (gum) disease. Because a periodontist combines advanced skills in treating gum disease as well as in dental implants, these patients are given a ‘leg up’ when it comes to treatment success.
In making your decision to opt for dental implants vs. crown-&-bridge, dentures or partials, it is important to understand the basics of how dental implants work. Although there are different types of implant systems, all work in in a similar fashion.
An implant is similar to a screw-like cylinder that is hollowed out in the center. This segment is what is placed into the bone to serve as a tooth root replacement.
Selecting the most appropriate type of implant and how many are needed is based on specific needs and goals. Our Western NC periodontal office plans for your placement procedure using computerized technology to determine the precise angles and depths for each implant before the placement procedure begins. This minimizes disruption to the gum tissues and bone structures, which in turn reduces healing time and optimizes comfort.
Once placed, each implant is covered over with gum tissue. For several months after, the implant goes through a process known as “osseo-integration.” During this phase, the bone grows around the implant, securing it into the bone. This recreates the foundation of natural tooth roots to give biting and chewing stability. Throughout this time, you can wear a denture or temporary so you are never without teeth.
Once healing is complete, a post is secured inside the hollow core of the implant. This post (or “abutment”) will support your final replacement tooth or teeth.
An important aspect of implant success also relies on the proper assessment of bone mass. When the upper or lower jaw has insufficient bone to support the implant being placed, there is a risk of failure.
Again, an implant requires careful selection and placement to be able to support the replacement teeth being attached. In some cases, as few as 4 – 6 implants can support a complete arch of teeth. This decision is best left in the hands of a periodontal specialist.
Severe bone loss can require bone rebuilding procedures prior to implant placement. This can be done by bone grafting or the application of a bone-rebuilding material. In some cases, dental implant systems designed with unique angles (such as the “All On 4”) can support a fulll arch of upper or lower teeth using minimal bone depth with no bone rebuilding necessary.
Another perk of the All On 4 is the forces of chewing and biting require only 4 implants on the upper and/or lower. Because implant costs are largely based on the number of implants placed, this can be a great savings for people who are candidates.
Why does successful placement rely so greatly on assessing bone mass? An implant must be placed in adequate bone that does not risk interfering with adjacent structures.
Without proper placement in sufficient bone, an implant risks coming in contact with a nerve that extends horizontally through the lower jaw. Upper implants placed too close to the sinus cavity can, over time, penetrate that area. Removing an implant in either of these situations, of course, is no simple task.
The ability to select the proper implant type for available bone depth is equally important.
Dental implant diagnosis and placement skills can vary greatly from one dentist to another. While some have taken extensive courses in implant dentistry, others may have taken a weekend course here and there. These are typically ‘hosted’ by a particular manufacturer who provides ‘training’ in a limited selection of implant types. In turn, this can limit the patient’s choices when relying on appropriate recommendations for his or her unique needs.
Obviously, a qualified doctor can enhance your potential for a successful outcome, which is where a periodontal specialist is a wise choice. A Periodontist has particular expertise in the diagnosis and placement of all types of Dental Implants. As a matter of fact, many general dentists prefer to have a Periodontist place implants in their patients. The patient then returns to their dentist for the attachment of teeth to the implants.
Rest assured – in our office, comfort is always a priority. For our patients, we offer oral or I.V sedation to accompany many procedures. While both are beneficial to calm anxiety, tension, stress or even intense feelings of fear, each has its advantages as well as limitations.
Oral sedation is in pill form and provides a fully relaxed state. It often erases most memory of the procedure after and has a quick recovery.
While oral sedation provides a very relaxed state, I.V. sedation puts you in a complete sleep state. This is sometimes referred to as “twilight sleep.” I.V. sedation is ideal for people with dental fear or phobia. This sedation is delivered through an I.V. drip, or intravenously. It takes effect rather quickly and patients nod off within minutes. This sedative erases memory of treatment afterward.
Whether given oral or I.V. sedation, comfort and safety are important to us at all times. And, while sedation is helpful when fear or anxiety exist, some people who have no fears at all request sedation for its ability to relax them during lengthy appointments.
While the doctor involved in your treatment is important, much of the potential for a successful result falls into the patient’s hands after the placement process. As a patient, having a successful outcome begins as soon as your implants are placed.
First, closely follow your post-placement instructions. For a few days following placement, most patients are advised to eat only cool, soft foods. This helps to minimize swelling and bleeding, which helps gum tissues to more quickly seal incision sites. This can lower your risk for infection.
Once home, other factors can also place your implants at risk. For example, smokers have a higher risk for implant failure. Because the chemicals in cigarette smoke are very drying to oral tissues, the healing process takes longer. Delayed healing creates a greater risk for infection to occur.
An element of risk that may surprise you is grinding or clenching teeth during sleep, which is typically a symptom of a misaligned bite. Some clenching is so intense the force can be likened to that used to crack a walnut. A sign of night-time clenching or grinding may be worn, chipped or broken teeth. However, even without signs, if you suspect you grind or clench, mention this to your implant dentist prior to treatment. This way, proactive measures can be taken to resolve the problem before complications result.
Most important of all is the patient’s commitment to maintaining good oral hygiene. Although Dental Implants themselves do not experience decay, the gum tissues and bone supporting the implants are as susceptible to oral bacteria as before. When oral bacteria infection (gum disease) penetrates to the implant site positions, the only way to treat the infection may require removing the implant.
In addition to being highly committed to your oral hygiene at home, your dental check-ups may be scheduled for every four months rather than twice a year. During these visits, a hygienist will remove accumulated oral bacteria to reduce risk to your Dental Implants. The condition of your gums will also be assessed.
Dental implants are designed to last a lifetime and are the closest thing to the natural teeth you once had. Too, the restored ability to bite, chew, speak and laugh without worry can be a tremendous boost to one’s self-esteem and self-confidence.
The type of dental implant best suited for you can be determined after an examination and review of x-rays (we use Cone-Beam digital imaging). Call 828-274-9440 to begin with a private, no obligation consultation to discuss your best options.
April is National Oral Cancer Awareness Month
Posted on Apr 12, 2022 by William J. Claiborne, DDS MS
April is recognized as National Oral Cancer Month. It provides an annual opportunity for the medical and dental communities to remind the American population of the dire consequences that can be brought on by this cancer.

Oral cavity and oropharyngeal (which includes the base of the tongue and soft palate) cancers occur most often in the tongue, gums, floor of the mouth, tonsils, and other parts of the mouth and oropharynx. These cancers also occur in the lips and salivary glands (typically those in the roof of the mouth).
According to the American Cancer Society’s, recent statistics of oral and oropharyngeal (throat) cancers include:
• In 2022, an estimated 54,000 new cases will occur with about 11,230 deaths.
• The average age of people diagnosed with these cancers is 63, but over 20% (1 in 5) of cases occur in patients under the age of 55.
• These cancers are more than twice as common in men as in women and slightly more common in white people than black people. Overall, the lifetime risk of developing oral cavity and oropharyngeal cancer is about 1 in 60 for men and 1 in 140 for women.
Although the death rate and new cases of oral cavity has risen only slightly over the past 20 years, there has been an increase specifically in oropharyngeal cancers associated with an human papillomavirus (HPV) infection in both men and women. These HPV-positive cancers tend to act differently than HPV-negative cancers.
A number of other factors can affect your risk for developing mouth and throat cancer. These include:
Tobacco and alcohol use – Tobacco use is one of the strongest risk factors for head and neck cancers, including oral cavity and oropharyngeal cancer. The risk for these cancers is much higher in people who smoke than in people who don’t. Most people with these cancers have a history of smoking or other tobacco exposure, like chewing tobacco. The more you smoke, the greater your risk. Smoke from cigarettes, pipes, and cigars all increase your risk of getting these cancers. Some studies indicate that long-term exposure to secondhand smoke might increase the risk of these cancers. 
Oral tobacco products (snuff, dip, spit, chew, or dissolvable tobacco) are linked with cancers of the cheek, gums, and inner surface of the lips. Using oral tobacco products for a long time is linked to a very high risk. These products also cause gum disease, destruction of the bone sockets around teeth, and tooth loss.
For people who continue to smoke and use oral tobacco products after cancer treatment, their risk of developing a second cancer in the mouth, throat, larynx (voice box), lung and other organs greatly increases.
Drinking alcohol increases the risk of developing oral cavity and oropharyngeal cancers. Heavy drinkers have a higher risk than light drinkers. Smoking and drinking alcohol together multiplies the risk of these cancers. The risk of these cancers in people who drink and smoke heavily is about 30 times higher than the risk in people who don’t smoke or drink.
Human papillomavirus (HPV) infection – HPV is a group of more than 150 types of viruses called papillomaviruses. Some of these viruses cause a type of growth commonly called a papilloma or wart.
Infection with certain types of HPV can cause some forms of cancer, including cancers of the penis, cervix, vulva, vagina, anus, mouth, and throat. HPV type 16 (HPV16) is the type most often linked to cancer of the oropharynx, especially those in the tonsil and base of tongue.
The number of oropharyngeal cancers linked to HPV has risen greatly over the past few decades due to becoming more common in younger people who have a history of multiple sex partners (including oral sex). This is true for even those with no history of alcohol abuse or tobacco use.
Gender – Oral cavity and oropharyngeal cancers are twice as common in men than in women. HPV-related oropharyngeal cancers are also seen more often in men.
Poor nutrition – Studies have found that a diet low in fruits and vegetables is linked with an increased risk of cancers of the oral cavity and oropharynx.
Being obese or overweight – Too much body weight appears to increase the risk of these cancers. It is advised that eating more plant-based foods, such as non-starchy vegetables and whole fruit, may help people lose weight as well as reduce their risk of oropharyngeal and laryngeal cancer.
Age – Because oral and oropharynx cancers can take many years to develop, they’re not common in young people. Most patients with these cancers are older than 55 when the cancers are first detected. HPV-linked cancers tend to be diagnosed in people younger than 50.
Sunlight – Cancers of the lip are more common in people who have outdoor jobs where they are exposed to sunlight for long periods of time.
Genetics – People with certain genes have a higher risk of mouth and middle throat cancer.
Signs and symptoms of mouth cancer may include:
• A lip or mouth sore that doesn’t heal within two weeks
• White or reddish patch on the inside of the mouth
• Loose teeth
• A growth or lump inside the mouth
• Mouth pain
• Ear pain
• Difficult or painful swallowing
Although oral cancer may first make itself known by a spot on the lips, inside of cheeks or on (or under) the tongue, oropharyngeal cancer can exist without symptoms. When symptoms do arise, they may be:
Mass felt in the neck or in the back of the throat
Difficulty or pain with swallowing
Muffled voice
Ear pain
Throat pain or sore throat
A periodontist is a dental specialist who has advanced skills in treatment involving the gums, including gum disease, gum reshaping and in the placement of dental implants. This specialist can also detect suspicious areas that may be early warning signs of oral or oropharyngeal cancer. Through a painless process, the examination can determine is a biopsy is needed for a thorough testing process. The earlier the treatment, the less involved the process will be. Too, early treatment helps to increase survival rates.
As an Asheville NC periodontal specialist, please react promptly to any signs or symptoms associated with these cancers. And, with this knowledge, make it your goal to share this information with a smile you love.
New Studies Reinforce Obesity-Gum Disease Connections
Posted on Apr 01, 2022 by William J. Claiborne, DDS MS
The first quarter of 2022 has concluded. If your New Year’s resolution to lose weight has waned by now, here’s an incentive to hopefully recommit to it. Researchers at Case Western Reserve University School of Dental Medicine recently conducted a study that found the human body with fewer fat cells is better able to combat periodontal (gum) disease. This is because fat cells trigger inflammation in the body.
In the study, 31 obese people who had clear indications of gum disease were monitored. Half of the group had gastric bypass surgery with fat cells removed from the abdomen. Those in the other group had not had gastric bypass surgery or fat removed.
Researchers noted that the majority of the bypass surgery group had a drop in their glucose levels following the procedure. This is a positive outcome based upon the higher risk of overweight people for diabetes and insulin-related problems.
All study participants underwent non-surgical periodontal treatments and were provided oral hygiene instructions for at-home care. While both groups showed improvement, the surgery group had better results.
https://www.sciencedaily.com/releases/2011/11/111109111540.htm
Inflammation in the body that continues without being able to resolve itself is known as systemic inflammation. This can have harmful effects over time, even eroding bone and that can lead to tooth loss. The inflammation can also cause breaks in the gums where harmful oral bacteria can enter the bloodstream. The potent bacteria of periodontitis (advanced gum disease) have been linked to preterm birth, stroke, heart disease, some cancers, diabetes and arthritis.
Years of scientific studies have long shown that insulin levels in diabetics improve when their gum health improves. Not surprisingly, the pathological processes that occur in both gum disease and rheumatoid arthritis (RA) are almost identical. Both have similar clinical structures, which are agents that cause disease or illness.
Based on the clinical makeup of gum disease and arthritis, the genetic similarity causes both conditions to cause chronic inflammation in tissues that connect to bone. It has also been shown that, by treating periodontal disease in RA patients, symptoms often improve. This has been attributed to a reduced burden of oral inflammation to the system.
Because excessive fat cells cause insulin to be more resistant to function as needed, a higher accumulation of sugar in the blood (hyperglycemia) occurs. By losing weight, insulin becomes less resistant and improves the diabetic status. Similar to improving inflammation levels in arthritic joints, gum disease treatment can also calm the inflammatory load from being overweight.
Another influencer of inflammation the researchers noted is the presence of the leptin hormone. This hormone is what regulates metabolism. Leptin has been linked to inflammation by increasing the production of a particular protein, which is also linked to inflammation (having a domino effect, of sorts). Because leptin production is reduced after bariatric surgery, the levels of inflammation are lower with better outcomes in periodontal treatment.
https://www.sciencedaily.com/releases/2021/11/211112083106.htm
In yet another recent study, the inflammation caused by obesity appeared to be a trigger for the development of cells that break down bone tissue. Natural teeth are held in place by the upper and lower jaw bone. To improve the understanding of the obesity-gum disease connection, research conducted at the University at Buffalo examined two groups of mice over a 16 week period. The mice were fed vastly different diets. The mice in one group were fed a low-fat diet (10% fat). In the other, the diet consisted of 45% fat, nearly half of that fed.
The high-fat diet group experienced obesity as well as higher inflammation and less bone mass where teeth are held in place. The researchers also noted that excessive inflammation resulting from obesity causes the cells that break down bone tissue. These cells, which originate in bone marrow, increase during illness in order to regulate immune function.
Bone loss is a leading symptom of gum disease, often leading to tooth loss. Gum disease affects nearly half of American adults ages 30 and older, according to the Centers for Disease Control & Prevention (CDC).
In NC, according to 2020 statistics, the CDC also reported that the obesity level of adults ages 30+ was 33.6. That’s one-third of our state’s population being obese. (https://www.cdc.gov/obesity/data/prevalence-maps.html#overall)
The relationship between the degree of obesity and gum disease is clear. However, as a periodontal specialist, I hope continued studies on the inflammation-bone connection that accompanies obesity (such as arthritis and osteoporosis) can improve the health of our U.S. population.
So, is the message here to improve your weight by improving your oral health? Research is certainly finding that one helps the other. After all, being at a healthy weight should make you smile, and we all want a smile that shows our confidence and overall well-being.
Know the common symptoms of gum disease and respond promptly by seeing a periodontist. Symptoms can include puffy gums that turn red in color; inflamed, swollen, or bleeding gums; gums that loosen from the base of teeth; persistent bad breath; gums that become spongy and bleed easily; and, pus pockets that form on the gums at the base of teeth.
If you are experiencing any of these, please contact our Asheville periodontal dental office. If dental fear of anxiety has prevented you from having regular dental care, we will be happy to discuss features such as oral and I.V. sedation (“twilight sleep”). Too, our office offers some of the most advanced dental technology in the Southeast. These options often save the patient much time in treatment, improve outcomes, and enhance comfort.
Call 828-274-8448 to begin with a consultation appointment. A referral is not necessary.