Header logo
header top contact widget
Blog Archives
Recent Posts
Categories
Archives
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- July 2014
- June 2014
- May 2014
- April 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- June 2012
Oral Bacteria Can Put An Immune System At A Disadvantage
Posted on May 20, 2021 by William J. Claiborne, DDS MS
Long before the COVID pandemic, it was widely known in the medical/dental and scientific communities that the bacteria in the mouth was intricately connected to the body’s overall health.
The oral cavity (interior of the mouth) contains some of the most varied and vast flora in the human body. It is the entryway for two systems vital to human function and physiology, the gastrointestinal and respiratory systems. Therefore, specific infections in the oral cavity may contribute to infection that can affect systemic health.
Systemic health refers to issues that affect the entire body, rather than a single organ or body part. An example of a systemic disorder is high blood pressure, which affects the body as a whole.
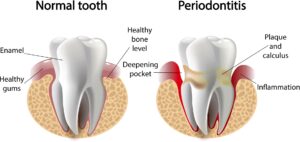
Research demonstrates that inflammation is a likely trigger for the systemic connection. For this reason, researchers have studied inflammation in the oral tissues caused by periodontal (gum) disease as a contributing factor of continual inflammation in the body.
 Hundreds of diseases and medications impact the oral cavity. Although the precise point of activation remains to be determined with some health problems, there is a more obvious association between oral bacteria and certain conditions.
Hundreds of diseases and medications impact the oral cavity. Although the precise point of activation remains to be determined with some health problems, there is a more obvious association between oral bacteria and certain conditions.
For instance, diabetes has a clear relationship with periodontal disease. Strong evidence shows that treating one condition positively impacts the other. By the same token, uncontrolled inflammation levels of one can worsen inflammation levels in the other.
Therefore, treating inflammation may not only help manage periodontal diseases but may also help manage other chronic inflammatory conditions.
Oral bacteria has been found to trigger or worsen other systemic conditions, including atherosclerotic vascular (heart) disease, pulmonary (respiratory) disease, diabetes, pregnancy-related complications, osteoporosis (bone loss), and kidney disease. A shared trait between gum disease and these medical conditions is that they are chronic conditions that take a long time to develop.
https://www.agd.org/docs/default-source/self-instruction-(gendent)/gendent_nd17_aafp_kane.pdf
According to the Centers of Disease Control & Prevention (CDC), nearly half of American adults ages 30 and over have gum disease – a whopping 47 percent. In a recent study, they found that about 9 percent have mild levels of gum disease, 30 percent have moderate levels and 8.5 percent have severe gum disease (periodontitis).
Researchers of a recent study found that 64 percent of adults ages 65 and older had either moderate or severe periodontitis. Gum disease rates were highest in males, Mexican Americans, adults with less than a high school education, adults below the poverty line and current smokers.
Although the initial stages of gum disease may be concealed behind the lips and cheeks, the interior of the mouth can signal the presence of periodontal disease at nearly every stage. For example, sore and swollen areas can indicate gingivitis, an early form of gum disease.
Worsening levels of gum disease can cause redness, tenderness, bad breath, bleeding when brushing, and receding gums. Progressive gum disease can lead to persistent bad breath, pus pockets forming around teeth, loosening teeth and painful chewing.
In your regular dental check-ups, your dental hygienist uses a “probe” to measure “pockets” along the base of teeth. During the exam, he or she measures the gum depth along each tooth – front, back and in-between. These depth measurements indicate areas where gum tissues have loosened from the base of teeth, and to what extent. The higher the number, the deeper the pocket.
 For example, healthy gums will measure 1 or 2. In some areas that are harder to reach when brushing or flossing, a 3 may be measured. However, a 4 or higher number indicates the gums are loosening their protective grip from the tooth. This leaves the tooth at risk for bacterial penetration below the gums.
For example, healthy gums will measure 1 or 2. In some areas that are harder to reach when brushing or flossing, a 3 may be measured. However, a 4 or higher number indicates the gums are loosening their protective grip from the tooth. This leaves the tooth at risk for bacterial penetration below the gums.
Healthy gums wrap snugly around the base of each tooth. This prevents the entry of bacteria, which can cause damage to the tissues and bone structures supporting tooth roots. Gum disease, to no surprise, is the nation’s leading cause of adult tooth loss.
However, infectious bacteria of gum disease don’t necessarily remain confined to the mouth. Through tears in diseased gum tissues, the bacteria are able to enter the bloodstream. Traveling through the body, these potent organisms can trigger reactions that activate or worsen serious health conditions.
For example, studies have indicated a relationship between periodontal disease and stroke. In one study focused on oral infection as a risk factor for stroke, people diagnosed with acute cerebrovascular ischemia showed a higher likelihood for having an oral infection than those who had healthy gums. (https://www.perio.org/consumer/gum-disease-and-heart-disease)
Along similar lines, men with gum disease have been found to be 49 percent more likely to develop kidney cancer, 54 percent more likely to develop pancreatic cancer, and 30 percent more likely to develop blood cancers.
Having healthy gums is actually easy – and rather inexpensive. Adults should brush thoroughly (at least 2 minutes) twice a day and floss daily. Snacking and sugar should be limited. The mouth should be kept moist throughout the day by drinking plenty of water (coffee, colas and tea doesn’t count). Moisture can also be replenished by the use of specially formulated oral rinses (available over-the-counter at many drug stores). By all means, drink alcohol moderately and avoid smoking.
Additionally, adults should maintain their 6-month dental check-ups and cleanings. These appointments help to remove any build-up of plaque or tartar on teeth so they are easier to maintain between visits. Too, your hygienist can point out areas of risk so you can concentrate appropriately during your at-home oral hygiene regimen.
If you’ve delayed (or avoided) regular dental care, your likelihood of having some level of gum disease is pretty high, even though you may not have obvious symptoms in early stages. Gum disease, once underway, does not go away on its own. It will gradually worsen and become a source of infectious bacteria that strains your immune system and increases your risks for serious health problems.
Begin with an examination appointment by calling our beautiful Asheville periodontal dental office at 828-274-9440. Here, we treat our patients with compassion, respect and with comfort a priority at all times. And, we provide patients with decades of experience and advanced skills — along with exceptional dental technology – so your treatment is successful and performed efficiently and effectively in minimal time.
While your smile is greatly important to your appearance, it’s what you can’t see that may harbor a rather ugly presence. Let’s get your smile in great shape!
Don’t Smoke? Living Or Working With A Smoker Creates Higher Risks Than Once Thought.
Posted on May 14, 2021 by William J. Claiborne, DDS MS
I doubt there is anyone in the U.S. who smokes tobacco who is unaware of the fact that it’s an unhealthy habit. Although the heart and lungs are more widely associated with the health risks of smoking, many people miss the fact that it is also damaging to the tissues in the mouth.
Consider the devastating statistics of COVID-19 related deaths in the U.S., nearing the 600,000 mark. Yet, when it comes to your oral health, cigarette smoking is responsible for more than 480,000 deaths per year in the United States. For people who don’t smoke but live or work with a smoker, secondhand smoke exposure accounts for over 41,000 of these.
For nonsmokers who are victims of secondhand smoke, that’s a tough statistic to accept.
Just how harmful is secondhand smoke? British researchers recently released some interesting findings along these lines. Their studies included several major countries and tracked nearly 7,000 adults, with nearly half being exposed to secondhand smoke. The findings showed that breathing in the smoke of another person’s cigarette can increase the risk of oral cancer by more than 50 percent. These cancers include lip, mouth and throat cancers.
On average, smokers die 10 years earlier than nonsmokers. For every person who dies because of smoking, at least 30 people live with a serious illness related to smoking. Smoking leads to disease and disability and harms nearly every organ of the body.
When considering the mouth, smoking can create costly problems in addition to a higher risk of tooth loss.
Twenty years of research shows that cigarette smoking is a risk factor for periodontitis. A smoker is 2 – 3 times as likely to develop periodontitis, which is an advanced stage of gum disease. In addition to increased prevalence, smokers also experience greater severity of gum disease.
Nicotine (in any form) has been shown to reduce blood flow in the gum tissues in the mouth. Pipe smoking can be worse than cigarettes due to the higher temperatures generated in the upper jaw. When it comes to dental implants, smoking is a risk factor for failure. It is also detrimental for conventional bridgework.
Cigarette smoking has long been associated with serious oral conditions, including periodontal (gum) disease, bone loss, tissue loss, and tooth loss. For smokers who opt for dental implants to replace missing teeth, they have a higher risk of peri-implantitis, which is inflammation of the soft and hard gum tissues surrounding a dental implant. To no surprise, smokers have a higher incidence of dental implant failure.
In an article published by the Journal of International’s Society of Preventive & Community Dentistry as far back as 2012, it warned that smoking can impact the rate of dental implant success, accounting for up to 20 percent of failures.
“Clinical trials of endosseous implants consistently rate smoking as a primary patient-centered risk factor for implant loss.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3894084/
It is common knowledge that the nicotine in cigarettes, e-cigs and ‘chew’ is an addictive drug. Some concerning quotes shared by the Oral Cancer Foundation are:
“Scientists have found that nicotine is as addictive as heroin, cocaine or amphetamines, and for most people, more addictive than alcohol,” states the article “Nicotine, Harder to Kick than Heroin,” published in the New York Times Magazine.
“Nicotine is similar in all critical measures to prototypic drugs of abuse such as cocaine, morphine and heroin.”
“Nicotine is a poison used as an insecticide.”
https://oralcancerfoundation.org/understanding/tobacco/tobacco-and-addiction/
Now, knowing the effects of secondhand smoke are likened to the non-smoking “victim” as inhaling half as many cigarettes as the user they live or work with, smokers should consider their habit in a different light.
While our Asheville periodontal dental office does not lecture or “guilt” our patients in any way, we feel they deserve to know the hazards of any risk factor related to the well being of their oral health. Without a doubt, smoking (whether cigarettes or vaping) is harmful to oral tissues and the potential to keep natural teeth.
In a report shared by Delta Dental, smokers are about twice as likely to lose their teeth than non-smokers, according to two 30-year studies at Tufts University in Boston. Their findings showed that men who smoke lose about 3 teeth for every 10 years of smoking, with women losing an average of 1.5 teeth per decade.
https://www.deltadentalins.com/oral_health/teethinpack.html
Every year, about half of smokers make some attempt at kicking the habit. Yet, only 6 or so percent are fully successful. All the while, the tobacco industry spends BILLIONS of dollars each year on cigarette and smokeless tobacco advertising and promotions.
According to the Centers for Disease Control & Prevention (CDC), in 2018 “$9.06 billion was spent on advertising and promotion of cigarettes and smokeless tobacco combined—about $25 million every day.” That’s more than $1 million dollars spent every hour of every day.
https://www.cdc.gov/tobacco/data_statistics/fact_sheets/economics/econ_facts/index.htm
While nicotine addiction means big money to the tobacco industry, it is enormously costly to our population. Now, knowing that secondhand smoke is so harmful to others, I hope our smoker patients will welcome our respectful support in their efforts to quit as we help them to maintain good oral health and keep their teeth (or dental implants) healthy for a lifetime of confident smiles.
If you’ve considered dental implants to replace missing teeth and smoke, please consult with us to discuss ways we can help you minimize the potential for dental implant failure. We want you to reap the benefits of a smile you’ll want to share proudly.
Call 828-274-9440 to schedule.
Your Tongue Is A Multi-Tasker!
Posted on May 05, 2021 by William J. Claiborne, DDS MS
 With the tongue occupying such a large area inside the mouth (or ‘oral cavity’), you’d think its anatomy would be common knowledge. Because this muscle functions continually without tiring, it tends to be taken for granted. It’s importance to your overall health, however, is unbounded.
With the tongue occupying such a large area inside the mouth (or ‘oral cavity’), you’d think its anatomy would be common knowledge. Because this muscle functions continually without tiring, it tends to be taken for granted. It’s importance to your overall health, however, is unbounded.
To correct a common misconception about the tongue, it is not the strongest muscle in the body. Although it ranks in the top 5 or so, the muscles surrounding the eyes actually have that supremacy. The heart, deemed the hardest working muscle in the body, and the masseter (jaw muscle) are also among those that are the body’s stand-outs.
The tongue does many things. It provides our sense of taste, is vital in pronunciation, moves food around as we chew, and aids in swallowing while helping to prevent certain things from being swallowed.
Not one muscle but a combination of 8, the tongue is coated with papillae. These are the tiny, bumpy protrusions on its surface. They help in various ways but are mostly credited for our sense of taste.
Different areas of the tongue are more sensitive to certain tastes. For example, the tip of the tongue detects sweet to the greatest extent while the sides detect sour. 
Papillae also sense touch so that we can feel the form and texture of food.
Saliva helps to keep the tongue moist so it can move around the oral cavity freely. Saliva is also helpful to the tongue by moving bacteria from its surface. However, saliva cannot keep the tongue bacteria-free.
Saliva and food residue can get stuck in the grooves between the papillae, especially on the last third of the tongue. This can create areas for bacterial growth. These bacteria thrive on remains of protein-rich food like fish, cheese or milk.
Here is where, as an Asheville periodontist, I have a particular interest in the tongue. As bacteria accumulate, a whitish film covers the tongue, which also causes bad breath. Keeping bacteria in the mouth to manageable levels is greatly supported by saliva flow.
The tongue’s underside covers two salivary glands of the lower jaw (submandibular glands). These ducts are located where the tongue meets the floor of the mouth.
If you’ve read some of my previous articles, you’ll recall that I’m constantly reminding readers of the hazards of having a dry mouth. Smoking, consumption of alcohol and caffeine, and many medications are all obstacles to the salivary glands being able to function efficiently.
A dry mouth provides a breeding ground for bacteria reproduction. When you consider the amount of bacteria embedded in the tongue’s surface, oral bacteria levels in the mouth can run rampant.
Because the tongue’s surface color can indicate too much oral bacteria, it should be looked at during at-home oral hygiene regimens. It is advised that, after brushing teeth, using the toothbrush to brush the tongue. This can dislodge an enormous amount of bacteria.
Although brushing the tongue tends to be done on the front area, it’s helpful to brush towards the back of the tongue where most bacteria exist (hence, the whiter color and smoother surface). Gagging will stop you from going too far so use that as a guide.
Some toothbrushes have a tongue scraper surface on the back side of the bristles. There are also tongue scrapers available for purchase. These are flexible strips that should be used to scrape from back to front 3 or more times after brushing. Rinsing the scraper is advised after each pass.
To provide even more support in helping the oral cavity control bacteria, an oral rinse can be very helpful. After brushing (for a minimum of 2 minutes) and flossing, swish for 30 or more seconds with an alcohol-free mouthwash. While the intensity of the mouthwash may be greater with initial use, most people notice its easier to swish around the mouth within a week or so.
Low bacteria levels in the mouth make for fresh breath and reduced risk of developing cavities and gum disease. Periodontal disease begins with gingivitis, which causes gum tissues to be tender and bleed when brushing.
Periodontitis, an advanced stage of gum disease, causes red, sore, spongy gums. Other symptoms are persistent bad breath, bleeding easily, gums that loosen from the base of teeth, and teeth that loosen.
Periodontitis can also cause health risks far beyond the mouth. Because these infectious bacteria can enter the bloodstream through tears in the gum tissues, it has been shown to trigger or worsen the development of serious health problems. Some of these are stroke, heart disease, arthritis, Alzheimer’s disease, some cancers, and diabetes.
When it comes to the tongue, remember its important role to your oral and overall health. Keep the mouth moist and its surface clean and your reward will be sweet (without the calories!).
If you are experiencing any signs of gum disease, call 828-274-9440 for an appointment. Gum disease does not go away on its own and will progressive worsen without treatment. Remember – it is the number one cause of adult tooth loss in the U.S.