Header logo
header top contact widget
Overall Health & Well-Being
Dental Fear?
Posted on Jun 25, 2015 by William J. Claiborne, DDS MS
It’s not surprising that the percentage of American adults with some level of dental fear (estimated at 75%) nearly parallels the percentage of adults ages 65+ who have some level of gum disease (70%), the nation’s leading cause of adult tooth loss.
The high number of adults who have dental fear is also likely related to the prevalence of tooth loss in mature adults. Those born before 1949 have the highest percentage of lost teeth and being totally toothless (25%). Could this be because the 65+ age group endured dentistry in a time when patient comfort was very different than what is expected today?
Most of today’s 35 and under adults have experienced dental care by modern dentists who are more attuned to a patient’s need for comfort. However, for adults in the 65+ age group, a greater number can recall traumatic experiences in the dental chair. These often carry over into adulthood, making a trip to the dentist overshadowed by the perception of pain.
Dental fear deters people from having regular dental check-ups. Lack of regular dental care leads to the formation of cavities, gum disease, tooth loss and health risks from oral bacteria, which can trigger systemic inflammation. The bacteria of periodontal (gum) disease can enter the bloodstream through tears in diseased gum tissues. The bacteria moves through the body, creating inflammatory reactions have been linked to heart disease, diabetes, stroke, arthritis, preterm babies and impotency.
For a large percentage of aging adults, dental fear plays a key role in the frequency of dental visits. If fear has kept you from regular dental visits, regardless of your age, you will find the majority of today’s dental environments are highly sensitive to your comfort throughout each visit. Although sedation options are an appealing way for fearful patients, we believe that finding a dentist or dental specialist whom you trust will help you conquer your fears and achieve the smile you desire.
Most patients who have avoided dental care have some level of gum disease. Until your gums are healthy, no dental procedure is going to provide long-term benefits. Begin with a periodontal exam by a specialist in Periodontics. Once your mouth is restored to a healthy state, we can make recommendations to help you with other needs for a confident smile.
Decades of dental fear isn’t going to disappear in a blink of an eye. Getting over it requires a pace you feel is right for you. If preferred, begin with a consultation appointment. Knowing you are empowered to control this pace may help you move through it comfortably.
Call (828) 274-9440 to discuss your needs or to arrange an appointment.
Why Tooth Loss Causes Your Jaw Bones To Shrink
Posted on Jun 22, 2015 by William J. Claiborne, DDS MS
The presence of natural teeth is vital to the health of upper and lower jaw bones. Tooth roots create stimulation to the bone, which stimulates blood flow so the jaws maintain a healthy mass. Without tooth roots, the lack of stimulation causes the bone to slowly decline. This process is known as “resorption.”
Resorption causes the gum ridge to flatten out over time, giving your denture a foundation that continually shrinks. Regardless of the amount of denture adhesive applied, the denture will begin to move while eating, causing uncomfortable rubbing. Laughing becomes overshadowed by the fear of embarrassing slips.
The pressure from wearing dentures actually accelerates resorption, especially for those who sleep in their dentures. The 24/7 pressure speeds the process of resorption to an even greater degree.
When dentures are first made, they may feel secure for the first five or so years. However, as resorption continues, relines help only on a temporary basis. As bone loss progresses, relines will last at less frequent intervals each time.
On average, denture wearers experience a 25% bone loss one year after natural teeth have been extracted. Three years later, 60% of the bone is gone. While natural teeth provide a biting force of 250 pounds, the average denture wearer bites with about 5 pounds of force.
Want to see the extent of bone loss you’ve experienced? Remove your denture and look in the mirror. Do you see deep wrinkles around the mouth? Do the corners of your mouth turn downward, even when you smile? Does your mouth appear collapsed inward with a pointed chin? Have jowls formed on the sides of your face?
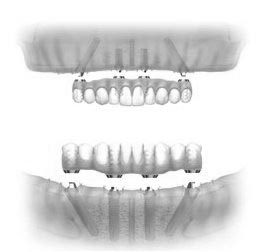
New designs in Dental Implant systems can overcome even severe bone loss. Types like All-On-4 can be placed in minimal bone using just four implants. Using specific angles, the All-On-4 system can support a full denture that is non-removable.
When a greater level of bone mass is necessary, procedures can restore the bone to a healthy level. Bone generating materials or a bone graft can be performed prior to implant placement. A “sinus lift” may be advised so sufficient bone exists between the upper jaw and sinus cavity.
Regardless of the procedure or implant type selected, a dental specialist who is trained and experienced in all implant types is the best choice for a successful result. A Periodontist is a dental specialist with advanced training in the diagnosis and placement of Dental Implants as well as bone rebuilding procedures.
Dental Implants restore chewing comfort and the ability to speak and laugh with confidence. Today, bone loss doesn’t necessarily prevent you from enjoying these benefits! Begin with a consultation by calling (828) 274-9440.
Connection Between Arthritis & Periodontal Disease
Posted on Jun 11, 2015 by William J. Claiborne, DDS MS
Rheumatoid arthritis (RA) is an inflammatory disease of the joints, affecting more than 1.3 million American adults. RA can lead to longterm joint damage, persistent pain and compromised function. Because RA can affect manual dexterity, oral hygiene routines at home can be difficult. Insufficient oral hygiene is the leading cause of periodontal disease, which, in turn, is the number one cause of adult tooth loss.
Research has indicated that RA sufferers have a higher incidence of periodontal (gum) disease compared to individuals with a healthy oral condition. Studies have also shown that RA patients are nearly 8 times more likely to have gum disease. However, researchers suspect that poor oral hygiene is not the only factor in an increased occurrence of gum disease in Arthritis sufferers. Study results have shown that while oral hygiene is a determining factor in acquiring gum disease, other parameters point to a deeper association between RA and gum disease.
Because both RA and gum disease create internal inflammation, a connection between the two makes sense. Inflammation is already suspected to be a correlating factor between periodontal disease and other conditions such as heart disease and diabetes. Even though research hasn’t proven a definitive gum disease-arthritis connection, findings increasingly show that periodontal disease doesn’t always occur as a result of RA, it may very well precede it.
The link between RA and gum disease are most prevalent when examining the joints and oral tissues. Oral tissues with the presence of periodontitis compared to tissues of RA-affected joints show a number of similarities. Research has also discovered a genetic link between the two.
Does oral bacteria trigger the development of arthritis? Does oral inflammation cause inflammation in the joints? While there is no definitive proof that one triggers the other, one study does show that treating periodontal disease can help in the prevention of RA. In a study of 40 people, with participants having both RA and gum disease, researchers found that those who who were given non-surgical gum disease treatment showed significantly more improvement in RA symptoms than those who were treated for RA only.
Of course, more research is needed to determine whether treating periodontal disease improves or even helps to prevent RA. In the meantime, people with RA should pay particular attention to oral health. If you have RA, caring for your teeth, both at home and through regular dental checkups, is important. If you have trouble caring for your teeth due to painful joints in the hands, ask your dentist or hygienist to recommend ways to overcome any challenges. Water flossers, electronic tooth brushes and oral rinses may make the task easier.
Although patients with RA are encouraged to maintain a diligent oral home-care regimen, it is highly recommended that any signs of gum disease be immediately treated by a periodontal specialist. These symptoms include gums that bleed when brushing, tender spots or pus pockets on gums, persistent bad breath, gum recession and gums that darken in color. It is also important that the oral care of RA patients is in coordination with their medical professionals.
Do you have Rheumatoid Arthritis? Begin by ensuring your oral health is at its best. A periodontist specializes in the care and treatment of oral tissues and is your expert in overcoming any level of periodontal disease. Call (828) 274-9440 to arrange a consultation.
Major Study On Connection Of Periodontal Disease & Cardiovascular Disease
Posted on Jun 01, 2015 by William J. Claiborne, DDS MS
As a Periodontal Specialist, I frequently read about research that shows a connection between the bacteria of gum disease and other severe diseases, such as heart disease. The connection makes perfect sense.
Largely unknown by the general population, gum disease bacteria can trigger inflammatory reactions elsewhere in the body. Oral bacteria has been associated with heart disease, high blood pressure, stroke, preterm babies, diabetes, arthritis, depression, and even impotency.
Although most infections are obvious, periodontal disease begins silently. Most people do not suspect it until a dentist or periodontist diagnoses it. The National Institutes of Health cites that nearly 75% of American adults have some level of periodontal (gum) disease.
A recent study on periodontal disease included more than 15,000 adults. Their dental health was monitored to determine if one’s oral health could be a risk marker for cardiovascular disease.
Of the 15,828 participants (all with chronic coronary heart disease), 16% had no teeth and 41% had less than 15 remaining teeth. Over one-quarter of the participants had gums that bled when brushing. According to the findings, as the number of remaining teeth declined, the higher the levels for heart disease and diabetes. There was also an increase in higher glucose and cholesterol levels.
While the exact link between oral bacteria and serious diseases is yet to be pinpointed, the evidence of an association has been overwhelming, thus far. It is known that oral bacteria is a definite part of the equation when it comes to heart disease. As research continues, we will share the findings on the link of one to the other.
One thing is certain – your oral health and overall health are connected. Protect both through a thorough regimen of oral hygiene at home along with regular dental check-ups. If you are experiencing symptoms of gum disease or are behind on regular dental care, call us at (828) 274-9440.
Recent Posts
Categories
Archives
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- July 2014
- June 2014
- May 2014
- April 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- June 2012